Key fact

233 million cases
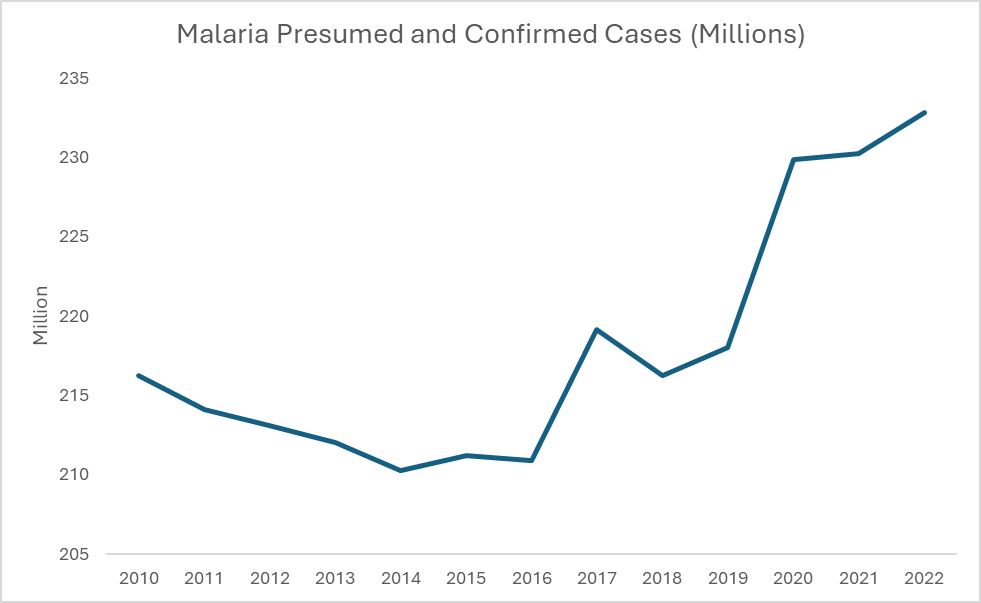
of malaria reported in the WHO African Region in 2022, compared to 234 million cases in 2021
Featured video
Globally, an estimated 2.1 billion cases and 11.7 million deaths were averted between 2000 and 2022. Most of the cases (82%) and deaths (94%) averted were in the WHO African Region.
- In 2022, 94% (233 million) of malaria cases reported in WHO African Region, compared to 234 million cases in 2021.
- In 2022, three countries in the African Region (Ethiopia: +1.3 million; Nigeria: + 1.3 million; and Uganda: + 597 000) bore the brunt of the global malaria case increases.
- In 2022, 95% of all malaria deaths (580 000) were in the WHO African Region, compared to 593 000 cases in 2021.
- Trends in the “High burden to high impact” (HBHI) countries (Burkina Faso, Cameroon, the Democratic Republic of the Congo, Ghana, India, Mali, Mozambique, Niger, Nigeria, Uganda and the United Republic of Tanzania) : Case numbers have largely stabilized in “High Burden to High Impact” (HBHI) since the pandemic, and the number of deaths is returning to 2019 levels. The 11 original HBHI countries represented 167 million cases (67% of the global total) and 426 000 deaths (73% of the global total), compared to 166 million cases and 430 000 deaths in 2021.
- Cabo Verde reported zero malaria cases for the fourth consecutive year in 2022 and has requested an official certification of malaria elimination from WHO (decision expected in early 2024)
Malaria remains a significant public health and development challenge. In 2022, the African Region bore the heaviest malaria burden, with 94% of cases and 95% of deaths globally, representing 233 million malaria cases and 580 000 of deaths, a small reduction compared to 2021.
The biggest challenge faced by malaria endemic countries in Africa is inadequate financing for malaria prevention and treatment services for people at risk of malaria. As a result, there are communities or populations that cannot access prevention measures or treatment when needed. In some parts of sub-Saharan Africa, mosquitoes that transmit malaria have become resistant to certain older insecticides.
Some people are more vulnerable to malaria than others. Partial immunity to malaria can be developed over years of exposure. As young children have not had the opportunity to build up this partial immunity, they are particularly at risk, and make up the majority of fatal cases of malaria in the WHO African Region.
As well as having a significant human cost, the effects of malaria extend far beyond direct measures of morbidity and mortality. Malaria can reduce school attendance, productivity at work, and there is evidence that the disease can also impair intellectual development. The economic costs are also significant. Between 1965 and 1990, countries in which a large proportion of the population lived in regions with malaria experienced an average growth in per-capita GDP of 0.4% per year, whereas average growth in other countries was 2.3% per year.
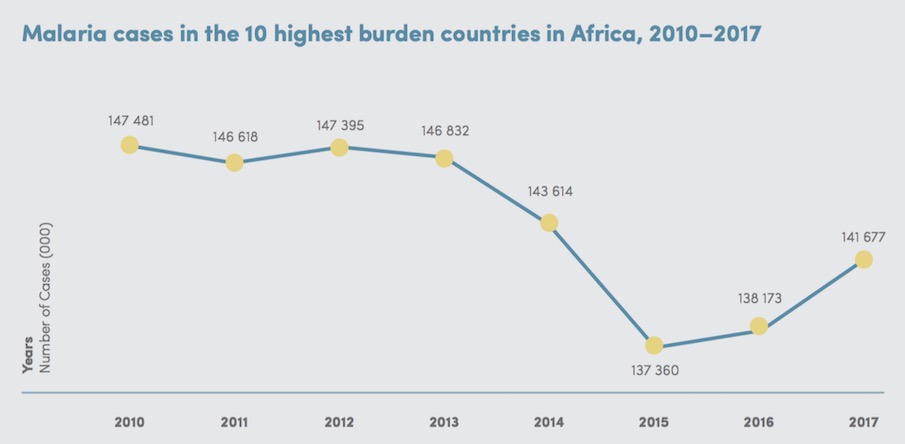
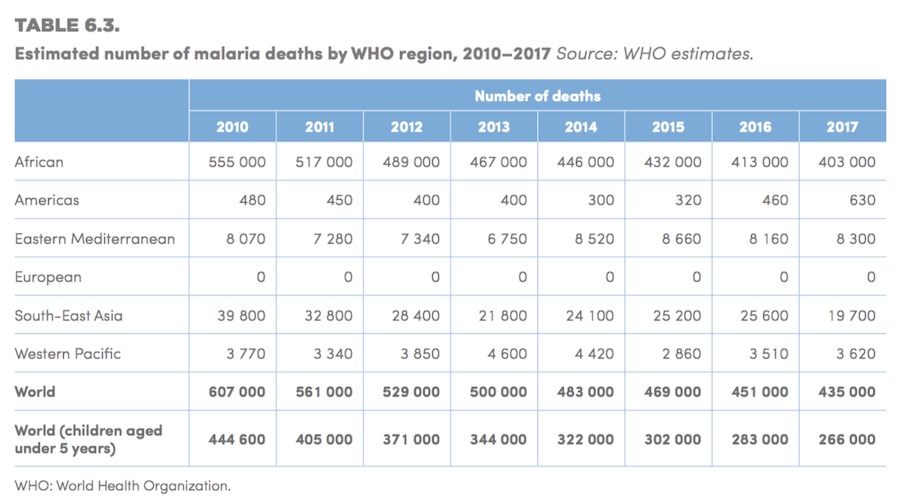
Disease burden
Malaria is widespread throughout tropical and subtropical regions of the world, and Africa carries a disproportionately high share of the global malaria burden, both in terms of total malaria cases and malaria deaths. In 2017, there were an estimated 219 million cases of malaria worldwide. Most were in the WHO African Region, with an estimated 200 million cases, or 92% of global cases. In 2017, five countries accounted for nearly half of all malaria cases worldwide. Four of these were in Africa: Nigeria (25%), the Democratic Republic of the Congo (11%), Mozambique (5%), and Uganda (4%).
Rationale
The WHO Global technical strategy for malaria 2016–2030, provides a technical framework for all malaria-endemic countries. It is intended to guide and support regional and country programmes as they work towards malaria control and elimination. The strategy sets ambitious but achievable global targets, including:
- reducing malaria mortality rates by at least 90% by 2030
- reducing malaria case incidence by at least 90% by 2030
- eliminating malaria in at least 35 countries by 2030
- preventing a resurgence of malaria in all countries that are malaria-free.
How far is the WHO African Region to achieve the above targets?
Key messages
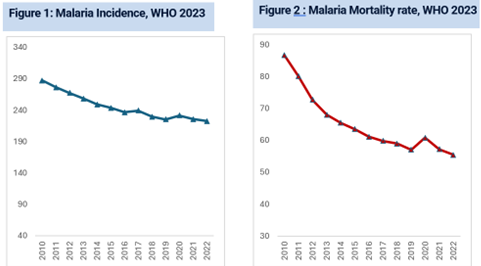
- Analysis of the trends shows that, in 2022, the WHO African Region was off track for both the malaria morbidity and mortality GTS milestones.
- In 2022, an estimated 580 479 people lost their lives due to malaria in the WHO African Region, which represented 95.4% of total deaths globally, including 78.1% of deaths in children under five compared with 90.7% in 2000.
- In 2022, an estimated 233 million cases of malaria in the WHO African Region, which represented 93.6% of total cases globally
- Between 2019 and 2022, there were substantial increases in estimated case numbers in Nigeria (5.3 million), Ethiopia (2.4 million), Madagascar (1.5 million), Uganda (1.3 million), the United Republic of Tanzania (1.3 million), Mali (1.1 million) and Mozambique (1 million). Over the same period, Rwanda saw a decrease of more than 3.8 million cases.
- Cabo Verde was certified malaria-free.
Reduction of malaria mortality rates
- The WHO African Region, with an estimated 233 million cases in 2022, accounted for about 94% of cases globally.
- Twenty-nine countries accounted for 95% of malaria cases globally. Four countries – Nigeria (27%), the Democratic Republic of the Congo (12%), Uganda (5%) and Mozambique (4%) – accounted for almost half of all cases globally.
Burden of malaria in pregnancy
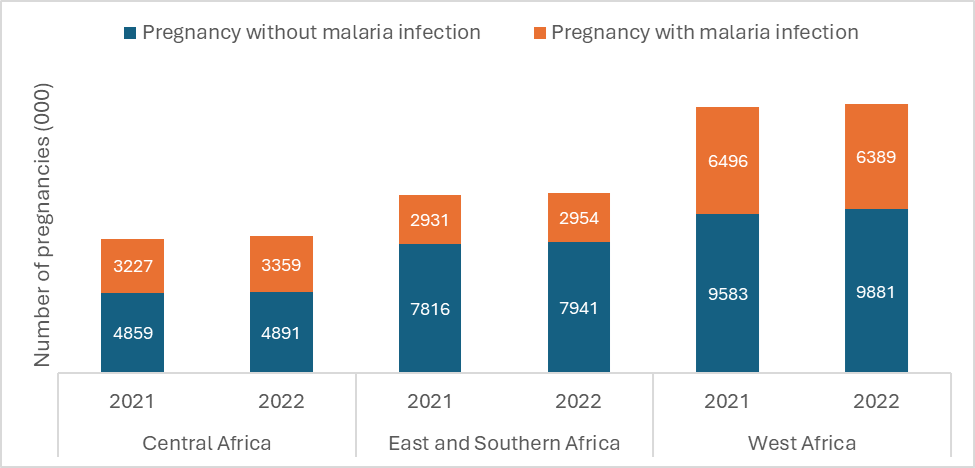
- In 2022, in 33 moderate and high transmission countries in the WHO African Region, there were an estimated 35.4 million pregnancies, of which 12.7 million (36%) were exposed to malaria infection during pregnancy.
- By WHO subregion, prevalence of exposure to malaria during pregnancy in 2022 was highest in west Africa (39.3%) and central Africa (40.1%), and lower in the east and southern Africa subregion (27.0%).
Malaria cases and deaths averted
- Globally, an estimated 2.1 billion malaria cases and 11.7 million malaria deaths were averted in the period 2000–2022.
- Most of the cases and deaths averted were in the WHO African Region (cases 82%, deaths 94%), followed by the WHO South-East Asia Region (cases 10%, deaths 3%).
Burden of malaria in pregnancy
- In 2022, in 33 moderate and high transmission countries in the WHO African Region, there were an estimated 35.4 million pregnancies, of which 12.7 million (36%) were exposed to malaria infection during pregnancy.
- By WHO subregion, prevalence of exposure to malaria during pregnancy in 2022 was highest in west Africa (39.3%) and central Africa (40.1%), and lower in the east and southern Africa subregion (27.0%).
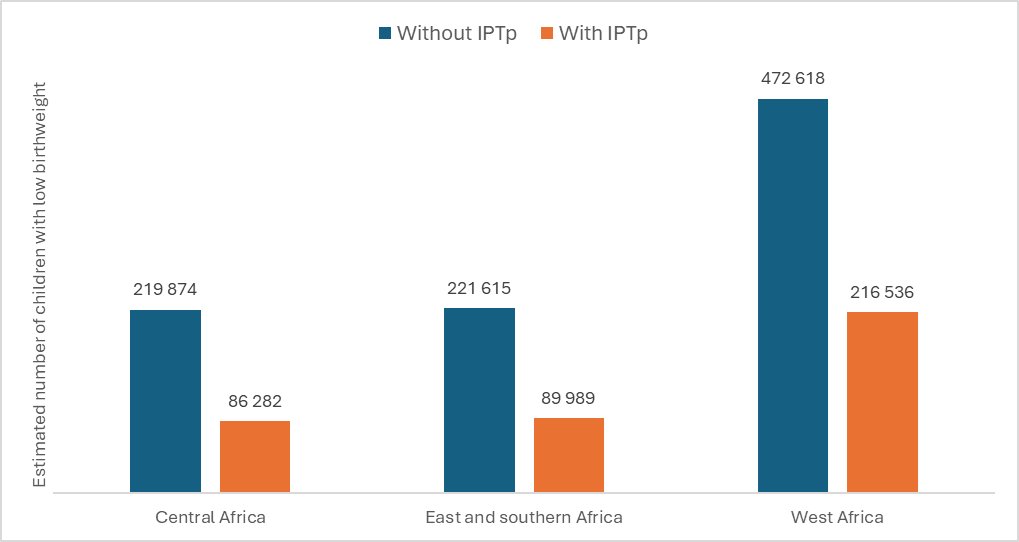
- It is estimated that, without a pregnancy-specific intervention, malaria infection during pregnancy in these 33 countries would have resulted in 914 000 neonates with low birthweight, compared with about 393 000 neonates with low birthweight estimated at the current intermittent preventive treatment during pregnancy (IPTp) coverage levels in the three subregions.
Malaria Elimination
- Over time, the elimination of malaria has gained momentum in numerous countries as they approach the milestone of zero indigenous malaria cases and as more countries are certified malaria free.
- Despite the setbacks, several countries and one territory saw notable reductions in indigenous transmission: Botswana (43.5%), the Democratic People’s Republic of Korea (9.3%), Ecuador (38.0%), Eswatini (57.6%), French Guiana (71.6%), Mexico (32.6%) and South Africa (31.3%).
Investments in malaria programmes and research
- The GTS sets out estimates of the funding required to achieve milestones for 2025 and 2030. Total annual resources needed were estimated at US$ 6.8 billion in 2020, rising to US$ 9.3 billion in 2025 and US$ 10.3 billion by 2030. An additional US$ 0.85 billion is estimated to be required annually for global malaria research and development (R&D) during the period 2021–2030.
- Governments of malaria endemic countries contributed more than a third of total funding in 2022, with investments of over US$ 1.5 billion, of which nearly US$ 0.4 billion was spent on malaria case management in the public sector and over US$ 1.1 billion on other malaria control activities. This was a substantial increase of over US$ 0.4 billion since 2021, largely stemming from an influx of domestic spending in the WHO African Region.
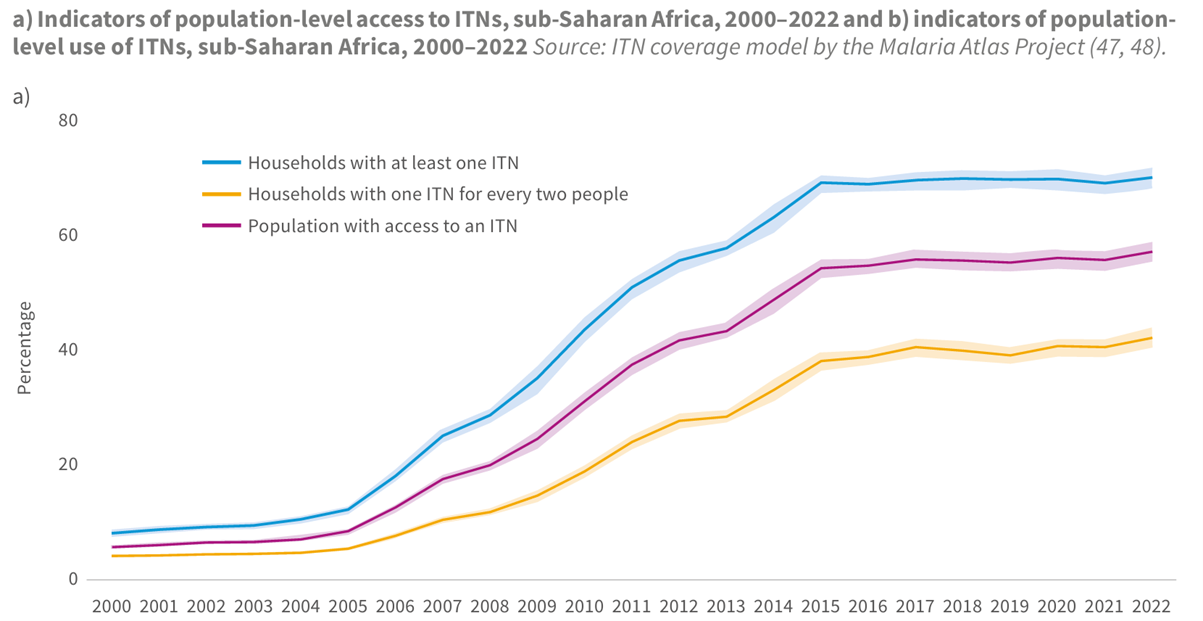
Distribution and coverage of malaria prevention
- By 2022, 70% of households in sub-Saharan Africa had at least one ITN, increasing from about 5% in 2000. The percentage of households owning at least one ITN for every two people increased from 1% in 2000 to 40% in 2022. In the same period, the percentage of the population with access to an ITN within their household increased from 3% to 56%.
Distribution and coverage of malaria diagnosis and treatment
- Globally, 3.9 billion rapid diagnostic tests (RDTs) for malaria were sold by manufacturers in 2010–2022, with 82% of these sales being in sub-Saharan African countries. In the same period, NMPs distributed 2.9 billion RDTs – 90% in sub-Saharan Africa.
|
Malaria cases and deaths averted
- Globally, an estimated 2.1 billion malaria cases and 11.7 million malaria deaths were averted in the period 2000–2022.
- Most of the cases and deaths averted were in the WHO African Region (cases 82%, deaths 94%), followed by the WHO South-East Asia Region (cases 10%, deaths 3%).
Malaria Estimated Cases In the African Region, WHO 2023
Estimated prevalence of exposure to malaria infection during pregnancy, overall and by subregion in 2022, in moderate to high transmission countries in the WHO African Region Sources: Imperial College and WHO estimate
Estimated number of children with low birthweight (WMR 2023)
Intervention
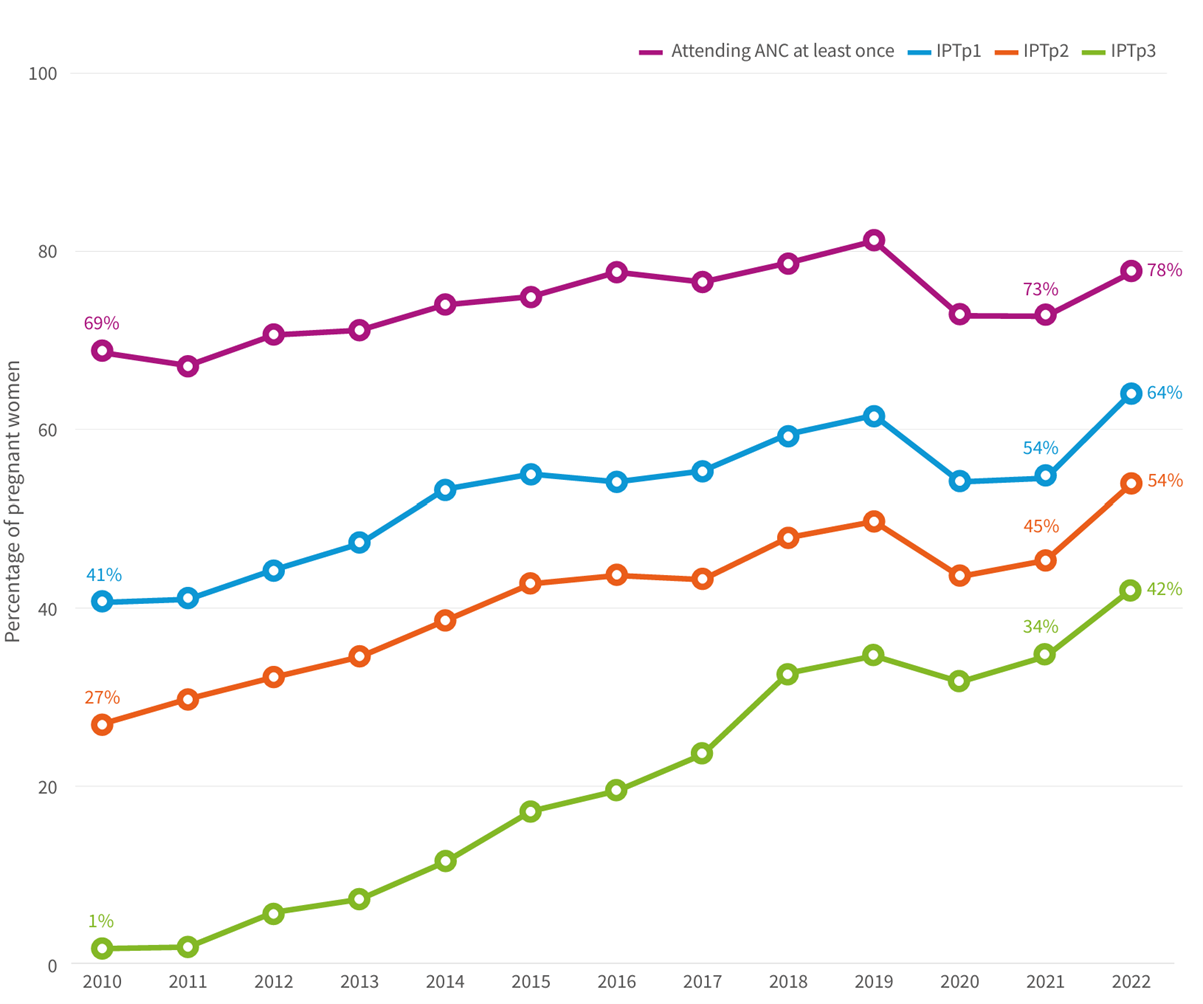
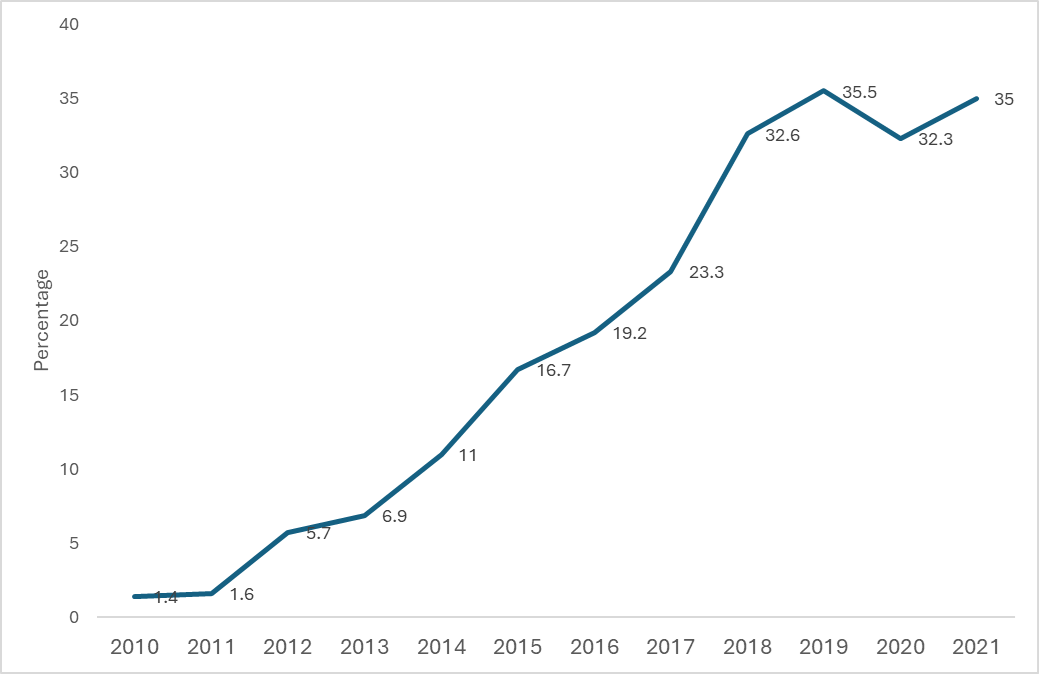
Pregnant women attending antenatal care at least once and receiving at least 3 doses of Intermittent Preventive Treatment of Malaria for Pregnant Women (IPTp3) (%) in the African Region, WHO 2021
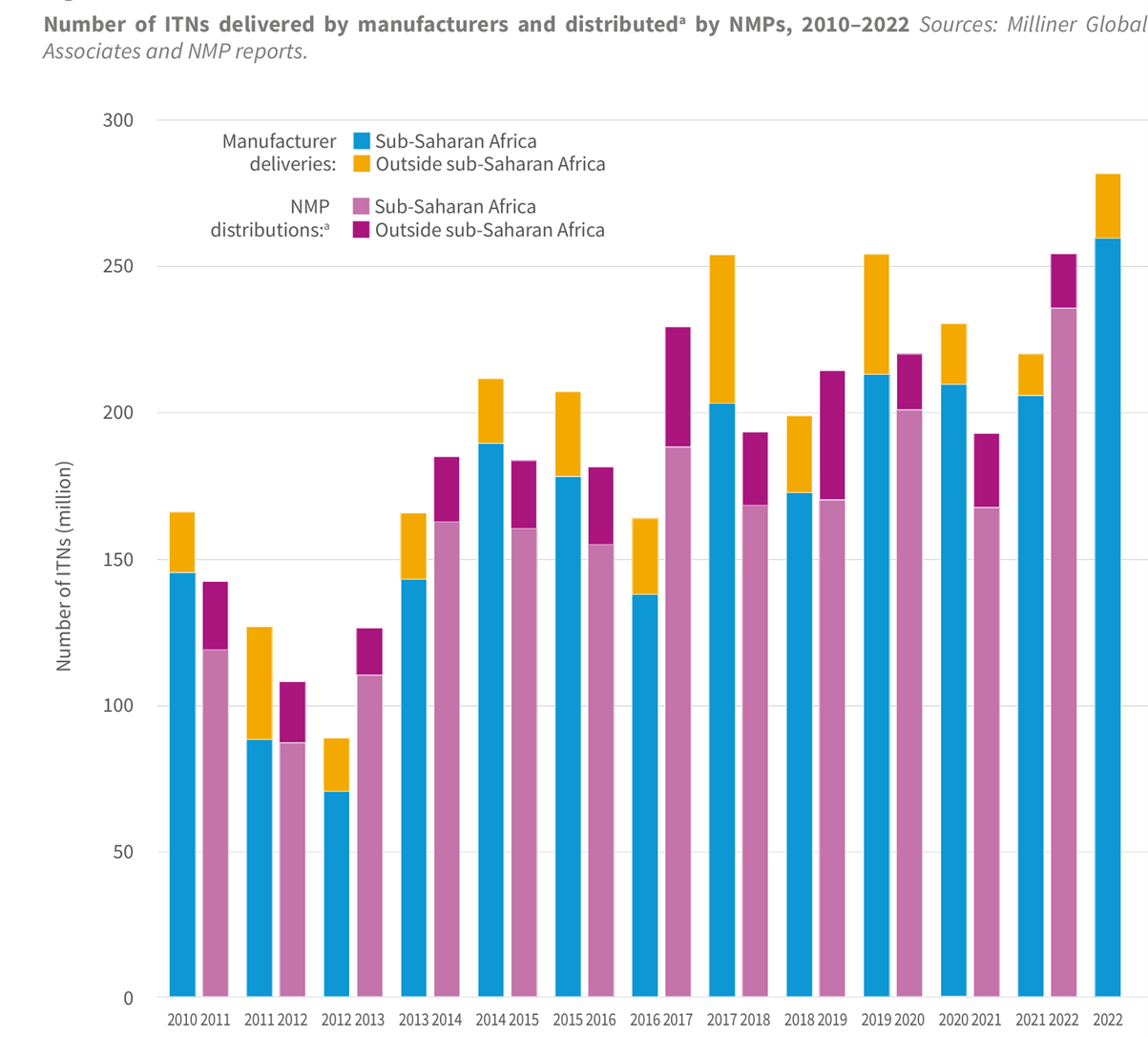
Number of ITN delivered by manufacturers and distributed by NMPs, 2010-2023
Indicators of population level access to ITNs, sub-Saharian Africa, 2000-2022 and b) indicators of population-level use of ITNs, sub-Saharan Africa, 2000-2022, Source; ITN coverage model by the Malaria Atlas Project.
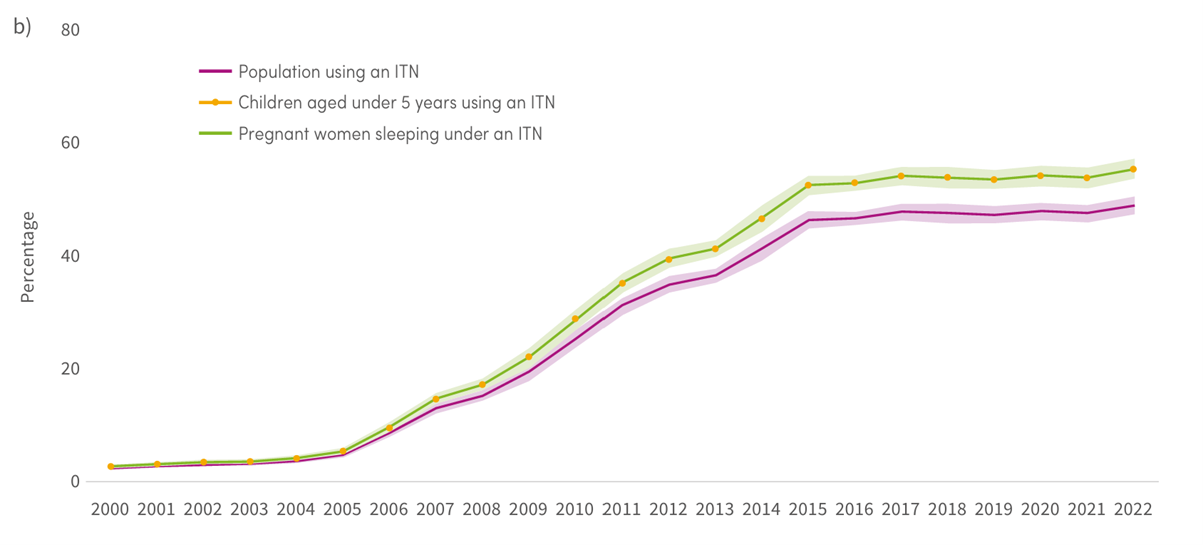
Indicators of population level access to ITNs, sub-Saharian Africa, 2000-2022 and b) indicators of population-level use of ITNs, sub-Saharan Africa, 2000-2022, Source; ITN coverage model by the Malaria Atlas Project.
Percentage of pregnant women attending an ANC clinic at least once and receiving IPTp, by number of SP doses, sub-Saharan Africa, 2010–2022 Sources: NMP reports, CDC and WHO estimates