Mbabane – Eswatini has made great strides in its response to HIV. New HIV infections have fallen steadily over the years, from 14 000 in 2010 to 4800 in 2020, and are projected to drop to 4300 by the end of 2023.
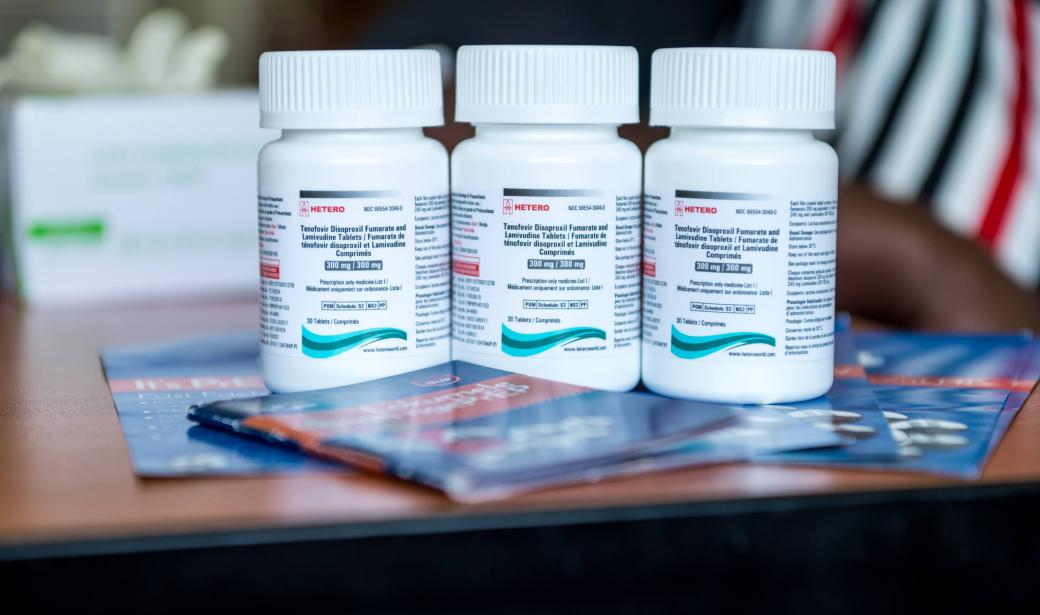
The country’s core set of HIV prevention strategies include increasing the uptake of high-impact services such HIV testing and counselling, HIV treatment, prevention of mother-to-child transmission, post-exposure prophylaxis, condom use and voluntary medical male circumcision. In 2018, the country piloted the rollout of pre-exposure prophylaxis, the use of an antiretroviral medication by HIV-negative people to reduce their risk of acquiring HIV.
With support from World Health Organization (WHO), Elizabeth Glaser Paediatric AIDS Foundation, the United States President’s Emergency Fund for AIDS Relief (PEPFAR), Georgetown University and other partners, the Government of Eswatini has bolstered the use of PrEP among people at higher risk of HIV infection it is now available from over 200 health facilities.
After discussions with the health workers, Dlamini decided she would take PrEP, in the form of an oral pill, to protect herself from HIV. For four years she has faithfully taken her medication. “I take PrEP always to be safe,” she says. “It makes me confident whenever I come to test knowing that I am negative.”
“We found that PrEP was feasible and acceptable, and also that expanding access encouraged more people to know their HIV status,” says Sindy Matse, Acting Programme Manager at Eswatini’s National AIDS Programme. “This provided an opportunity for clients to discuss individual risks, and increased understanding and awareness of HIV risk.”
Faith Mamba, a midwife at Siphocosini clinic in Hhohho District receives routine refresher trainings from these partners. The last training was on how to administer event-driven PrEP, which is effective in reducing the likelihood of men acquiring HIV during sex. A man takes oral PrEP for approximately three days before anticipated sex.
“I feel valuable,” says Mamba. At least I help somewhere. I always encourage people to use protection despite using PrEP.”
The number of PrEP users is on the rise, from 2200 in 2018 to 32 750 clients in 2022, surpassing the target of 20 000 clients for that year. And the number of health facilities providing PrEP rose from just 22 in 2017 to 204 in 2022.
Dlamini is positive about these innovations in HIV prevention. “The vaginal ring would be nice since the clinic sometimes experiences drug stock outs,” she says. “Also, women want to be part of new innovations, like how men can use event-driven PrEP two hours before having sex.”
For now, Dlamini is happy to continue to take her pill. She says her family knows that she uses PrEP and that she will continue to take the pill. “To remain negative for as long as I can,” she affirms.
Shirley Amimo
Work cell: +26876195916
World Health Organization Eswatini
2nd Floor, UN building Somhlolo Road, Mbabane.
Media Relations Officer
WHO Regional Office for Africa
Email: dalalm [at] who.int
Tel: +254 703 245 761 (WhatsApp)