WHO provides technical support, develops policies, guidelines, standard recording and reporting forms, health promotional materials, and coordinates control and research efforts. WHO brings together all major actors involved in Buruli ulcer on a regular basis to share information, coordinate disease control and research efforts, and monitor progress.
WHO provides antibiotics to endemic countries to ensure access to treatment free of charge for all patients.
WHO supports worked towards three research priorities:
- understand the mode of transmission
- develop rapid diagnostic tests
- establish best-case antibiotic treatments.
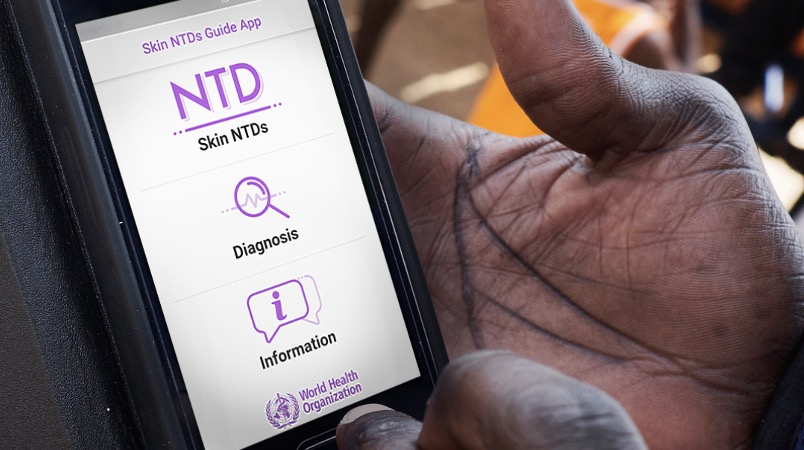
Online courses and a Skin App for Android and iOS to assist health workers in the field in the diagnosis of skin NTDs including Buruli ulcer.