Improving access to mental health services in Sierra Leone
Mental health service delivery remains challenging in Sierra Leone and critical gaps in staffing mean thousands are unable to access the services they need. Steps are now being taken to increase psychosocial support available within communities and health facilities.
With a population of 7,000,000 people, Sierra Leone only has two psychiatrists, two Clinical Psychologists, and 19 Mental Health Nurses. Just four nurses have specialized in Child and Adolescent mental health.
In order to bridge this gap, the Ministry of Health and Sanitation is working together with its partners to strengthen the delivery of mental health services in the country, aiming to roll out psychosocial training for various levels of staff at health facility as well as community levels.
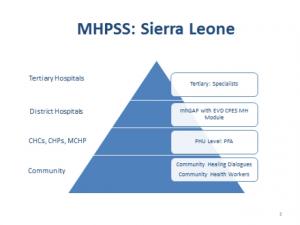
At the Community level, there will be training for at least two social workers and two nurses per district to organize and facilitate Community Healing Dialogues, which help communities identify coping resources and mechanisms and provide mutual support for psychosocial problems. The dialogues will engage 15 to 18 community members, meeting once every week to discuss and promote mental health issues in their communities. Additionally, community health workers will be trained to identify people with mental disorders, how and where to do referrals as well as home visits and to support patients and carers.
At the next level, health care workers will be trained in Psychological First Aid to help them to recognize distress symptoms in themselves and in their colleagues and to be better able to recognize signs of distress among patients.
Further to this, community health workers and medical doctors distributed around the country will be trained on the mental health gap action programme (mhGAP). The mhGAP is an approach developed by WHO for supporting mid-level and higher level health care workers to provide more specialised mental health services. They will be able to use simple procedures to assess for mental disorders, determine diagnosis identify possible treatment options. It has been very widely used and evaluated in other countries in the African region.
The ultimate goal is to also have professionals who provide more specialized care at the main referral hospitals including the Kissy Psychiatric National Referral Hospital, Connaught Hospital and Ola During Children’s Hospital. Currently, only Connaught has a Psychiatrist, working with King’s Health Partners.
WHO in collaboration with other partners, is providing technical support to strengthen mental health services within the Ministry of Health and Sanitation to improve the quality of care for people in need of help. Specifically, support is being provided for the review of the 1902 “Lunacy Act”; the review of the Mental Health Policy and Strategic Plan, training of health care workers in Psychological First_Aid, training of 120 Community Health Officers in WHO Mental_Health Gaps Action Programme as well as in rolling out Community Healing Dialogues.