Progress report African region 21 - 2.10. Vaccination

At the cusp of a mass vaccination roll-out, with support and guidance from WHO, at least 40 African countries started vaccination planning before sufficient COVID-19 vaccines became available. Despite advocacy on the part of WHO and its partners in public health, a regional vaccination roll-out during the first six months of the year fell short of expectations. However, some countries made use of WHO’s COVID-19 Vaccine Country Readiness Assessment Tool, and managed to vaccinate priority populations such as the elderly, health care workers and those suffering from preconditions. Despite the vaccine supply crunch, seven countries, including Equatorial Guinea, Mauritius, Morocco, and Seychelles had reached by end July vaccination rates significantly above the continental average. In addition, about 30 countries have used more than three quarters of the vaccines received.
To reach at least 30% of the population by year-end, WHO-AFR and its partners estimate that 780 million vaccines would be required for Africa. Encouragingly, whereas only 245 000 doses were supplied to just six countries in June, by July commitments to improve vaccine access and distribution began to materialize. By the end of the reporting period, 3.8 million vaccine doses were delivered to 13 countries through the COVAX Facility, bringing the total doses delivered to the continent to 82 million. These recently delivered vaccines are part of 60 million doses COVAX has allocated to 49 African countries, scheduled for delivery between July and September. However, with associated costs – distribution, personnel, logistics, and equipment hovering at US$ 5.00 for every US$ 1.00 spent on a vaccine –, at the time of writing this report, funding for the entire vaccination effort on the continent had not yet been resolved.
To increase Africa’s capacity to address vaccine shortfalls more efficiently, WHO and its partners have advocated for domestic production of the COVID-19 vaccine, and a patent waiver for vaccines. As a result of these efforts, and following a loan from the United States, South Africa – the country with the largest number of cases on the continent – began vaccine production in June 2021. This initiative aims to produce 400 million doses of COVID-19 vaccines for the African market, which are set to be distributed by 2022. COVAX has also sealed deals with Sinopharm and Sinovac to supply 32.5 million vaccine doses to Africa. Allocated during the last week of July, these doses are scheduled for delivery as soon as countries are ready to receive them.
Ghana, the first African country to receive vaccines through the COVAX Facility, reached over 470 000 people in areas of highest prevalence of COVID-19 cases in just 20 days. This included some 60% of its first-phase target population, and around 90% of all health care workers. Ghana’s strategy was to ‘pre-list’ populations through mapping, screening, and scheduling appointments for vaccinations in advance. Such a strategy was instrumental to the world’s most rapid and well-targeted COVID-19 vaccination roll-outs. Strong logistical preparations and coordination were key to reaching people in remote areas in the country. To vaccinate elderly people living in hard-to-reach communities, Ghana’s mobile vaccination teams received strong backing from community mobilizers.
In a similar manner, Angola’s electronic pre-registration system helped ensure the right people were vaccinated and that they were aware of where and when to get the vaccine. SMS messaging, email confirmations and QR codes for on-site verification have also proven useful in preparing to deliver second doses, as well as collecting data to monitor the safety of vaccines. Angola vaccinated 70 000 people from priority groups across the country, half of whom were health care workers. In addition, the country invested in cold chain logistics and storage facilities to ensure that all COVID-19 vaccines, including those which must be stored in ultra-cold temperatures, will remain usable.
Mauritius, Rwanda and Seychelles, all of which had held wide-ranging vaccine roll-out simulation exercises in advance, achieved a strong rate of vaccination by the end of July. With support from WHO AFRO, several countries had conducted simulation exercises by mid-July, most possessing strong regulatory and safety procedures. This support enabled countries to secure personal protective equipment (PPE) for vaccination teams which made infection prevention a key part of the vaccine roll-out, in addition to training and supervision of the teams for safe vaccination delivery.
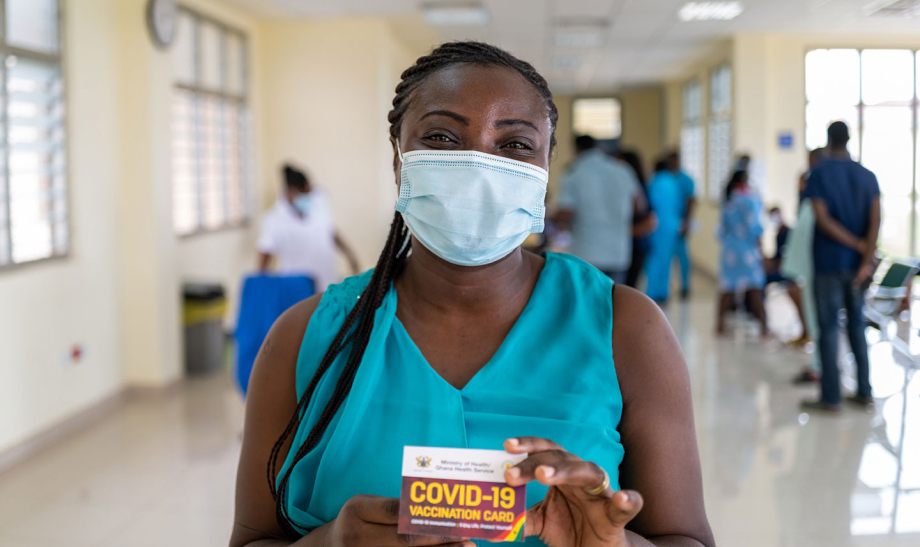
WHO / Blink Media – Nana Kofi Acquah
Falsified vaccines
WHO-AFR deployed specialists, conducted trainings, and workshops in at least 40 countries to address weak regulatory systems, and to curb the expansion of falsified and substandard drugs and vaccines, along with false information and marketing. Countries took part in infodemic management and social listening exercises. A communication guide to explain the efficacy and safety of the Chinese manufactured Sinopharm and Sinovac was widely disseminated, to dispel misinformation regarding the alleged poor quality of those vaccines, as compared to other market brands.
What are the main challenges for Africa’s COVID-19 vaccine roll-out?
COVID-19 vaccines are just one part of the response, but vaccine supply constraints pose a serious threat to the health and welfare of people on the African continent.
I would like to amplify the call from WHO to those countries that have already vaccinated their high-risk populations to share their excess doses. Many African countries are struggling and we cannot afford to wait until late 2022 to only protect our high-risk groups. Let us remember the world is interconnected, and that if Africa lags behind, there will be implications for the rest of the world.
The unpredictability of supplies demands an agile approach to the vaccine roll-out from us, and our teams are on high alert to assist countries around the clock. More delays in vaccinations will only exacerbate the emergence of new variants of the virus.
Having said that, if it hadn’t been for the COVAX Facility, many African countries wouldn’t even have the small number of doses they have received so far.
Dr Messeret Shibeshi
Immunization Officer

Dr Messeret Shibeshi
How COVAX Works:
COVAX is a partnership between the World Health Organization (WHO) and two international groups – Gavi, the Vaccine Alliance and the Coalition for Epidemic Preparedness Innovations (CEPI) – which aims to send vaccines to developing countries, with UNICEF as the main logistics partner. Most COVAX funding comes from high-income countries and organizations such as the Bill & Melinda Gates Foundation. At the summit of the G7 industrial nations in May, leaders announced a contribution of 850 million doses to the scheme. Another important collective vaccine initiative is the African Union’s African Vaccine Acquisition Trust (AVAT). It is managed by Africa CDC, and in July UNICEF signed an agreement with Janssen Pharmaceutica NV to supply up to 220 million doses of the J&J single-dose vaccine to all 55 Member States of the African Union (AU) by the end of 2022. Some 35 million doses are to be delivered by the end of this year. Several African countries have purchased vaccines, or have negotiated bilateral vaccine donations from producing nations.

OCHA Sudan




