Report of the Regional Director 21 - Chapter 1
Report of the Regional Director - 2021 - Chapter 1

Responding to COVID-19
and other emergencies,
and investing in preparedness
Every three days, Member States report an acute health event to WHO in the African Region; 80% of these are outbreaks and most are of zoonotic origin. In addition to the devastation caused by COVID-19, African countries have battled outbreaks of Ebola, yellow fever, measles and other diseases, as well as humanitarian crises. As WHO, we have worked with countries to strengthen capacities to prepare for, prevent, detect, respond to, and quickly recover from emergencies.
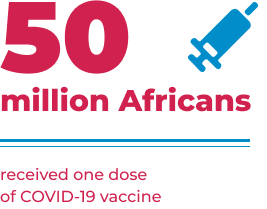
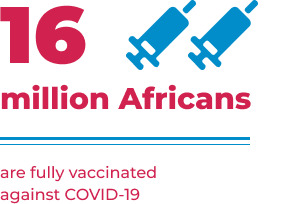
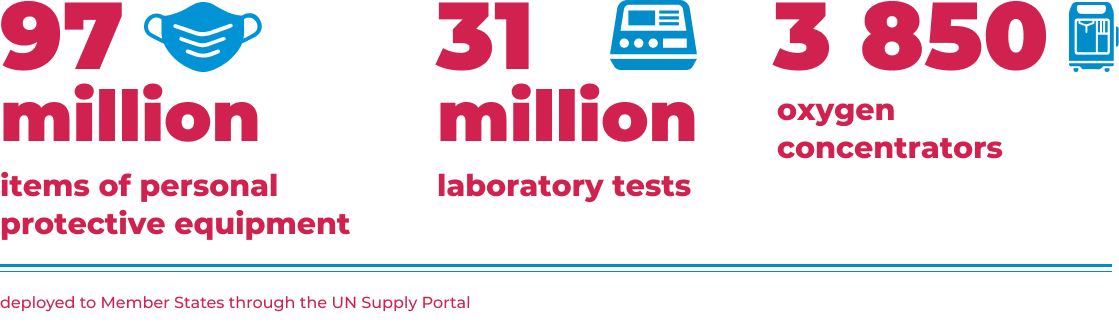
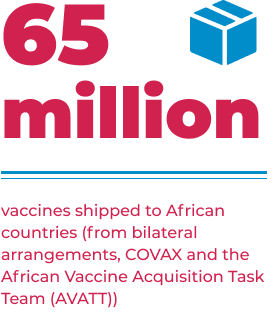
Key achievements in the COVID-19 response in the African Region






Report on the Strategic Response to COVID-19 in the WHO African Region: February–December 2020
Timely and effective response to health emergencies
In the past year, WHO supported countries in the African Region to respond to 50 public health emergencies. The WHO Incident Management System has been activated within 48 hours for all major events. This included 46 WHO graded emergencies triggering WHO procedures and activities to support the management of the response.1 More than 2000 experts across multiple disciplines were deployed to African countries to support response operations. To ensure a coordinated response to humanitarian emergencies, there are 12 active national health clusters bringing together operational partners.2
In the past year, WHO supported countries in the African Region to respond to 50 public health emergencies.

Forty-one Member States have functional public health emergency operations centres and WHO is providing support to improve the operations of incident management systems, including guidance documents,3 in-depth training and technical support for seven countries4, and weekly webinars with over 5000 national responders participating.
Thirty-three countries implemented health logistics services including establishing severe acute respiratory infections (SARI) treatment centres, screening points, community facilities and distribution of 3097 beds to health facilities. Two Intra-action reviews of the UN Supply Portal were also conducted and found gaps in coordination at country level, lack of visibility and predictability of order status and lead times. Recommendations to address these shortcomings are being implemented.
Building stronger clinical care capacities
will have long-term benefits for health
The COVID 19 pandemic has placed a huge stress on already strained health systems in the African Region but to help reduce this, WHO deployed supplies, equipment, and guidance to countries to enhance case management for COVID-19. More than 50,000 doctors and nurses were trained in all countries.
Since the start of the pandemic, supplies and equipment worth 123 million dollars have been shipped to African countries. These investments have gone a long way in building capacities to manage moderate and severe COVID-19 cases.
Investing in critical care capacities in African countries now, will pay dividends for the COVID-19 response, along with strengthening health systems to manage other major causes of severe illness and death. This will result in health and development gains for generations to come.
Ebola outbreaks in Guinea and
the Democratic Republic of the Congo
11th Ebola outbreak in Equateur Province
in the Democratic Republic of the Congo
1 June – 18 November 2020
130
cases
55
deaths
75
survivors
40 000
vaccinated
12th Ebola outbreak in North Kivu Province
in the Democratic Republic of the Congo
7 February – 3 May 2021
12
cases
6
deaths
6
survivors
1 898
vaccinated
Nzerekore region in Guinea
14 February – 19 June 2021
23
cases
12
deaths
10
survivors
10 898
vaccinated
More than 100 experts were deployed by WHO to the Democratic Republic of the Congo and Guinea to support response operations. Through the Contingency Fund for Emergencies (CFE), US$ 860 000 and US$ 2.2 million were released to support operations in the two countries respectively.

Crisis response in northern Ethiopia
The humanitarian crisis in the Tigray region of northern Ethiopia has resulted in an estimated 1.7 million people internally displaced, 62 000 refugees in neighbouring Sudan and 2.8 million in need of health assistance. The conflict has disrupted access to water, sanitation and health services, health supplies and commodities including essential drugs.
US$ 2.2 million from the WHO CFE and US$ 2 million from the UN Central Emergency Response Fund (CERF) have been released to scale up operations to respond to the health emergency in Tigray.
WHO in collaboration with partners has deployed mobile health assistance teams covering 67 of the 93 targeted woredas. The health resources and services availability mapping system (HeRAMS) found that of the 205 health facilities in Tigray, only 40 were fully functional. All centres urgently needed more medical supplies, drugs and equipment. Nutrition kits to treat 1500 cases of severe acute malnutrition with medical complications (SAM-MC) and 1250 trauma kits including materials and drugs to meet the needs of 50 acutely injured patients requiring surgical care in emergency situations were delivered to accessible areas. The kit is designed for use in areas where basic levels of infrastructure exist. WHO deployed 23 experts to the response. US$ 2.2 million from the WHO CFE and US$ 2 million from the UN Central Emergency Response Fund (CERF) have been released to scale up operations to respond to the health emergency in Tigray.Crisis response in Cabo Delgado, Mozambique
Since October 2017, waves of violence have affected Cabo Delgado in north eastern Mozambique, leading to internal displacement of over 710 000 people, and 2.7 million facing severe acute food insecurity. The situation has been exacerbated by recurrent climatic shocks, cholera and COVID-19. WHO has deployed 17 experts to provide technical and operational support, and delivered supplies to manage 1500 cases of cholera and provide emergency care for 10 000 people for three months. Health workers in all treatment centres in Cabo Delgado and Nampula Provinces have been trained in clinical management of cholera.
Preparing for all hazards
The COVID-19 crisis has clearly demonstrated and underscored the need for investments in preparedness. The pandemic has overwhelmed even well-resourced countries, highlighting the dividends of preparedness and international solidarity for all countries.
In recent years, WHO has worked with 34 countries5 to develop national action plans for health security, based on the findings of joint external evaluations of each country’s capacities under the International Health Regulations (IHR, 2005) and other preparedness assessments. Funding to implement these road maps should be a top priority as countries recover from COVID-19.
The pandemic has overwhelmed even well-resourced countries, highlighting the dividends of preparedness and international solidarity for all countries.
As COVID-19 cases started to spread globally in early 2020, WHO facilitated a readiness assessment in the African Region. This helped to kick-start the development of national COVID-19 preparedness and response plans, the activation of whole-of-government coordination mechanisms, prepositioning of supplies, and mobilization and training of multidisciplinary responders.
WHO convened pattern coordination meetings early on, which resulted in the creation of technical working groups through the WHO emergency hubs in Dakar and Nairobi. These groups brought partners together to provide context-specific guidance to Member States across all pillars of the COVID-19 response.
The sentinel surveillance network for influenza in the Region was leveraged to rapidly scale up COVID-19 polymerase chain reaction (PCR) testing capacity from 32 countries with PCR capacity for influenza to all 47 countries in the Region.

More than 2300 people from 15 countries6 were trained using the African Region Risk Communication and Community Engagement “5 steps package”.7 This information was then cascaded to communities to equip thousands of people with the knowledge to prevent COVID-19 and to combat misinformation around the virus and vaccines.

Readiness levels were regularly monitored through an online information system, and an organization-wide Incident Management Support Team (IMST) was established at the Regional Office by mobilizing staff from all departments to effectively provide day-to-day support to all 47 Member States. This team worked with WHO teams at the subregional, national and district levels and with partners, to provide comprehensive support to national authorities in leading response operations.
27 countries conducted intra-action reviews at national and subnational levels with WHO support. The findings from these assessments were used to adjust response strategies and for peer learning.
To document lessons learnt during the COVID-19 response and to identify and address gaps, 27 countries conducted intra-action reviews at national and subnational levels with WHO support.8 The findings from these assessments were used to adjust response strategies and for peer learning.
A dashboard was developed to track the public health and social measures implemented in response to COVID-19, and to share information among IHR States Parties. Member States were also guided on risk-based implementation of these measures to reduce their socioeconomic impacts.
For the fourth consecutive year, Member States in the African Region maintained 100% annual reporting of their IHR capacities. Hazard-specific plans were also developed for the 10 African countries9 in the meningitis belt and 10 countries10 prone to cholera outbreaks.
Implementation of the third edition of Integrated Disease Surveillance and Response (IDSR) technical guidelines was enhanced through development of an online training course on the OpenWHO platform and the establishment of communities of practice. Forty-six countries11 are implementing IDSR, including 2112 with at least 90% coverage at subnational level. Thirty countries have adapted the revised guidelines at the national level and 44 have conducted IDSR training.
Point-of-entry readiness capacities were enhanced through peer review, capacity-building workshops and cross-border collaboration meetings involving 27 countries. Seven virtual cross-border meetings were held in relation to epidemics of Rift valley fever, yellow fever and Ebola, bringing together 10 Member States in West Africa13 to improve information sharing and collaboration.
Point-of-entry readiness capacities were enhanced through peer review, capacity-building workshops and cross-border collaboration meetings involving 27 countries.
In East and Central Africa, cross-border collaboration to manage COVID-19 cases among truck drivers led to arrangements for pre-departure testing and certification, sharing of movement itineraries, number of persons travelling in vehicles, and awareness of COVID-19 preventive measures. This helped to limit cross-border COVID-19 transmission.
Assessing risks and sharing information
The availability of relevant, timely information is crucial to guide preparedness activities and response operations. Using the Epidemic Intelligence from Open Sources (EIOS) platform, 118 signals were detected and verified in the past year, of which 12 new acute events were identified in 11 countries. Across all countries in the Region, 158 acute public health events were monitored and 15 rapid risk assessments were conducted.14
To manage the massive demands for information on the COVID-19 pandemic as well as outbreaks of Ebola, WHO has developed a dynamic-layered data management system bringing together different information sources and datasets, with epidemiological analysis to produce regular information products (Figure 1). An operational tool to regularly assess risk levels across countries was also developed.
Fig 1: COVID-19 Information Flow in the WHO African Region

Several dashboards have been created to bring together key pieces of information. The WHO COVID-19 dashboard has recorded over 1.3 million visits. In addition, a regional Ebola website was created with dashboards for the Democratic Republic of the Congo and Guinea. All-in-one geographic information system (GIS) online dashboards have been developed for COVID-19 for six countries15 and trained data managers are maintaining them. More than 3000 static maps describing acute health events have been created and shared.
The Weekly Bulletin on Outbreaks and Other Emergencies reaches over 6000 people, and an internal COVID-19 situation report is being published daily since March 2020. Guidance documents16 developed during this period have contributed to improved contact tracing and targeted interventions. Collaboration with the Tackling Infections to Benefit Africa (TIBA) partnership, Association Action en Santé Publique in Switzerland and the South African Centre for Epidemiological Modelling and Analysis allowed in-depth analysis of the evolution of the pandemic and its potential trajectory in the Region, thus informing prevention and mitigation measures.
COVID-19 statistics published through various social media platforms have reached more than two million people a day with 50 000 engagements.
- The 12 graded emergencies were: COVID-19 in all Member States; Chikungunya in Chad and Congo; cholera in the Democratic Republic of the Congo; dengue in Côte d'Ivoire; hepatitis E in Burkina Faso and Namibia; measles in the Central African Republic and Democratic Republic of the Congo; poliomyelitis in 17 Member States; Rift valley fever in Mauritania; and yellow fever in Guinea.
- Such as the United Nations Children’s Fund, the International Organization for Migration, the International Federation of Red Cross and Red Crescent Societies, Médecins Sans Frontières, the Medical Devices Agency, the United Nations High Commissioner for Refugees, and Save The Children.
- Public Health Emergency Operations Center (PHEOC) Legal Framework Guide: A Guide for the development of a legal framework to Authorize the Establishment and Operationalization of a PHEOC and (ii) Handbook for Public Health Emergency Operations Center operations and management.
- Botswana, Burundi, Eswatini, the Gambia, Namibia, Niger and Zimbabwe.
- Benin, Botswana, Burkina Faso, Burundi, Cameroon, Central African Republic, Chad, Comoros, Côte d’Ivoire, Democratic Republic of the Congo, Eritrea, Ethiopia, Eswatini, Ghana, Guinea, Kenya, Lesotho, Liberia, Malawi, Mali, Mauritania, Mozambique, Namibia, Niger, Nigeria, Rwanda, South Africa, Senegal, Sierra Leone, South Sudan, Uganda, United Republic of Tanzania, Zambia and Zimbabwe.
- Algeria, Benin, Burkina Faso, Burundi, Cabo Verde, Cameroon, Comoros, Côte d'Ivoire, Guinea, Guinea-Bissau, Madagascar, Mauritania, Niger, Senegal and Togo.
- The five steps are: RCCE system; internal and partner coordination; community engagement; public communication; rumour and disinformation management.
- Angola, Botswana, Burkina Faso, Cameroon, Democratic Republic of the Congo, Eswatini, Ethiopia, Gabon, the Gambia, Guinea, Lesotho, Liberia, Malawi, Mauritius, Mozambique, Namibia, Niger, Nigeria, Rwanda, Senegal, Sierra Leone, South Africa, South Sudan, United Republic of Tanzania, Uganda, Zambia and Zimbabwe.
- Benin, Cameroon, Chad, Côte d’Ivoire, Eritrea, Ghana, Mali, Niger, United Republic of Tanzania and Togo
- Benin, Democratic Republic of the Congo, Ethiopia, Kenya, Mozambique, Nigeria, South Sudan, United Republic of Tanzania, Zambia and Zimbabwe.
- Except Algeria
- Angola, Burundi, Chad, Comoros, Côte d'Ivoire, Gabon, the Gambia, Guinea, Lesotho, Liberia, Mali, Namibia, Niger, Nigeria, Rwanda, Senegal, Seychelles, Sierra Leone, South Africa, Togo and Uganda
- Côte d'Ivoire, the Gambia, Guinea, Guinea-Bissau, Liberia, Mali, Mauritania, Niger, Senegal and Sierra Leone.
- Three of which were for COVID-19 (including two global rapid risk assessments and the variant of concern in South Africa). Rapid risk assessments were also conducted for Ebola virus disease in Democratic Republic of the Congo and Guinea, yellow fever (Guinea, Senegal and Nigeria), hepatitis E (Burkina Faso), Rift Valley fever (Mauritania), acute jaundice syndrome (Burkina Faso), Chikungunya (Chad), monkeypox (Democratic Republic of the Congo) and plague (Democratic Republic of the Congo).
- Congo, Democratic Republic of the Congo, Ethiopia, Liberia, Sierra Leone and Togo
- (i) Technical Guidance for Contact Tracing for COVID-19 in the WHO African Region and (ii) Guidance Document for a Differentiated Response to COVID-19 Outbreak in Urban and Rural Settings.


