Report of the Regional Director 21 - Chapter 2
Report of the Regional Director - 2021 - Chapter 2

Supporting continuity
of essential services and
sustaining gains in health
- Strategic action to improve access to quality essential health services
- Better health for women, children, adolescents, and older people
- Mitigating the impacts of COVID-19 on supplies and strengthening regulatory systems
- Investing in health workers – heroes of the COVID-19 response
- Building sustainable financing systems and ensuring financial risk protection
Past, severe epidemics – for example, Ebola outbreaks in which more people died of malaria than Ebola – have highlighted the importance of sustaining access to other life-saving services. Learning from these experiences, continuity of essential services has become a key pillar of emergency response operations, including the COVID-19 response.
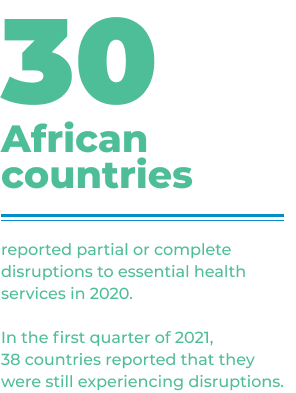
Two global WHO pulse surveys on continuity of essential health services have been conducted during the COVID-19 pandemic, first between May and July 2020, and then in the first quarter of 2021. The results of these surveys showed disruptions across all service areas, and most frequently those for mental health, immunization and chronic conditions like diabetes and hypertension. The reasons varied from population fear of visiting health facilities to movement restrictions, and drastic changes in workforce capacity due to redeployments or COVID-19 infection.
This highlights the importance of improving access to quality care towards attaining universal health coverage. Throughout the COVID-19 crisis, WHO has been working with African countries to strengthen health systems using integrated, people-centred approaches.

Strategic action to improve access to quality essential health services
The formulation and review of national health plans is becoming more inclusive and designed towards ensuring the availability and quality of health services. Ghana, Guinea, Niger and Nigeria were supported to develop national plans to ensure the continuity of essential health services during the COVID-19 pandemic. Technical assistance was provided to seven countries1 for the development of new strategic plans with a focus on UHC through primary health care (PHC). UHC scoping missions were conducted in Mauritania and Sao Tome and Principe to advocate for a coordinated approach towards strengthening primary health care-oriented health systems towards UHC.
Better health for women, children, adolescents, and older people
Countries have implemented a range of good practices to ensure the continuity of essential services and minimize disruptions during the pandemic:
- Developing national guidelines, protocols, and tools for service continuity.
- Reorganizing service delivery approaches: for example, in Uganda, smaller antenatal care (ANC) groups were formed, down from 10 women to groups of two or three. Tips on preventing infections were also shared. These actions helped to increase the trust of pregnant women in ANC services.
- Multi-month dispensing of contraceptives and medicines for chronic diseases, such as three- to six-month supplies of antiretrovirals, to reduce the frequency of health facility visits and decrease the risk of exposure.
- Task sharing: for instance, in Cameroon, community health workers were authorized to prescribe iron tablets for pregnant women. This brought basic quality health care closer to the population and reduced congestion in health facilities.
- Public-private partnerships: in South Africa, the ride-share application, Uber, provided victims of violence with free transport to and from courts, health facilities and shelters.
- Promoting self-care interventions such as depot-medroxyprogesterone acetate subcutaneous (DMPA-SC) self-injected contraception.
- Strong stock management by establishing eLogistics Management Systems (ELMS) to facilitate real-time monitoring of supplies and avoid stock-outs.
- Monthly monitoring of service provision
- Mobilizing communities, involving youth, women’s and faith-based groups and traditional leaders to support dissemination of health promotion and disease prevention messaging.
- Using digital technologies: for example, in South Africa, MomConnect, a free artificial intelligence-based messaging service was used to convey information to pregnant and postnatal women.
- Communications about where and how to access services using different channels, such as mobile applications, radio, television, social media, youth networks, faith-based groups, and district task force meetings.
The regional Reproductive, Maternal, Newborn, Child and Adolescent Health Technical Advisory Group (RMNCAH TAG) was launched in November 2020. This group brings together independent experts to advise WHO on how to accelerate progress in preventing deaths among women, adolescents and children, and to improve sexual and reproductive health in the Region. Countries were also supported to develop plans to improve RMNCAH2, to promote healthy ageing3, and to advance sexual and reproductive health and rights.4

Key regional training packages and tools5 were updated in line with WHO recommendations, including those on promoting a positive pregnancy experience, uterotonic use in labour, breastfeeding, kangaroo mother care, and care of small or sick newborns. Nine countries developed training curricula on service integration, to update information in key areas such as gender-based violence, family planning, and prevention of mother-to-child transmission of HIV.
Webinars attracting more than 10 000 health workers, and virtual launch and awareness-raising events were held to aid the dissemination of this new information. For example, the newly launched WHO Labour Care Guide (WHO Next Generation Partograph) was shared with more than 1500 national and provincial programme managers and health workers across 38 African countries. Over 3300 nurses and midwives were oriented on the guidance.
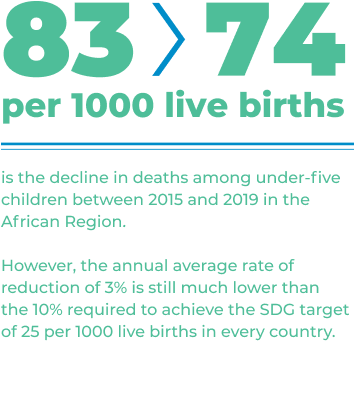
Most childhood deaths are due to preventable and/or treatable conditions for which effective interventions exist. Coverage of existing child survival interventions has shown some improvement but remains unacceptably low in the African Region.
The Network for Improving Quality of Care for Maternal, Newborn and Child Health supported four countries6 to develop guidelines and digital tools to maintain essential services, monitor service quality, and engage communities. Countries were also supported to implement quality of care road maps,7 adopt standards for maternal and newborn health8 and complete quality of care assessments.9
WHO is working with youth organizations in Kenya and Zimbabwe to tailor messaging around COVID-19 preventive measures, including vaccine acceptance, as well as participation of young people in decision-making bodies. After six years of implementation, an evaluation of the Ministerial Commitment on comprehensive sexuality education (CSE) and sexual and reproductive health services for adolescents and young people in Eastern and Southern Africa was conducted.
It showed that political will and engagement on adolescent sexual and reproductive health and rights had increased, accompanied by accelerated legal and policy developments. This resulted in a 4% increase in knowledge among young people about preventing sexual transmission of HIV. The Region recorded a decrease of 37 640 new HIV infections among young people between 2015 and 2019. Based on the evaluation findings, joint UN advocacy briefs were developed to assist UN agencies and partners with advocacy on issues related to the harmonization of ages of consent.
Mitigating the impacts of COVID-19 on supplies and strengthening regulatory systems
With disruptions to the global supply chain, all countries have strengthened capacities in forecasting and monitoring, particularly of commodities needed for the COVID-19 response and continuity of essential health services.
The pooled procurement initiative for Small Island Developing States was signed by the Ministers of Health of the seven countries concerned10 on 29 September 2020. The prequalification of suppliers has been completed, the list of priority medicines finalized, the regulatory requirements harmonized and the secretariat is assisting the Member States on sourcing and price negotiation.
Four countries11 revised their national medicines policies, and five countries12 updated their national essential medicines lists, promoting the optimal use of antibiotics through the WHO AWaRe categorization, and prioritizing medicines to be manufactured, supplied, prescribed and dispensed for equitable access to essential services.

Blood donations decreased by 17%, while blood demand and transfusion both dropped by 13%.13 To sustain blood collection, countries invigorated voluntary blood donor networks. So far, only 16 countries14 have national haemovigilance systems in place and in the past year Burundi and Zambia were supported to establish these systems. Twenty countries15 built capacities in establishing these systems. In collaboration with the West African Economic and Monetary Union (UEMOA), eight countries16 developed blood regulatory systems and Gabon was supported to train staff of the National Blood Transfusion Services on safe blood donations including categorizing blood donors. Countries also developed blood safety strategic plans,17 and road maps to improve access to safe blood products.18
Surveys in six countries on substandard and falsified medicines showed that only 57% of antibiotics tested were in compliance with international quality requirements.
Surveys in six countries19 on substandard and falsified medicines showed that only 57% of antibiotics tested were in compliance with international quality requirements. This suggests that the prevalence of substandard and falsified medicines in Africa is four times higher than the global benchmark. Training on substandard and falsified products was included in the pharmacy curricula in five countries.20 In the reporting period, WHO issued an alert on falsified retinol (vitamin A) detected in Chad.
Two other falsified products, Fluzone® Quadrivalent Influenza Vaccine and COVID-19 Vaccine BNT162b2, were identified in the WHO Region of the Americas. To guarantee access to quality-assured medical products, Member States need to reinforce national frameworks to prevent, detect and respond to substandard and falsified products in partnership with law enforcement and border control authorities, using risk-based quality surveillance, stringent product traceability, and increased investment in regulatory capacity and infrastructure.
Together, WHO and Africa CDC set up the Regional Expert Advisory Committee on Traditional Medicine for COVID-19 to elevate the standards of clinical trials, including by pooling expertise for multicentre studies. Trials of traditional medicines for COVID-19 are now at phases I and II in several countries.21
Manufacturing medical products in the African Region
With imports accounting for 70% to 90% of medical products consumed in Africa, it is time to scale up local production. In line with the African Union’s Pharmaceutical Manufacturing Plan for Africa, WHO collaborates with the United Nations Industrial Development Organization (UNIDO) and the United Nations Economic Commission for Africa (UNECA) to stimulate local manufacturing of pharmaceuticals.
To reduce dependence on imported medical products, African leaders expressed their will to boost local manufacturing capacity. WHO responded to these requests from Africa and other regions by establishing a world local production forum. The forum was held for the first time from 21 to 25 June 2021 and brought together decision-makers from governments, industry, academia and the international community. It facilitated vivid discussions on key issues surrounding local production and technology transfer among countries and partners. Algeria, Ethiopia, Ghana, Kenya, Nigeria, Rwanda, Senegal and South Africa have embarked on the road towards setting up manufacturing facilities for vaccines and participated in the transfer of production know-how.
The quality and prices of manufactured products constitute two pivotal elements, which ensure long-term sustainability of local pharmaceutical manufacturing. WHO’s support in the areas of regulatory system strengthening, harmonization and convergence was instrumental in ensuring that national regulatory authorities would play their part in guiding industry towards manufacturing excellence and would help ensure conformity of their products with international standards. Going forward, WHO is working with South Africa, and discussion has started with Rwanda and Senegal to establish messenger RNA hubs for technology transfer for the production of COVID-19 vaccines. WHO stands ready to continue assisting countries with technology transfer, building their regulatory expertise and facilitating private sector partnerships needed for the success of local production.
Investing in health workers – heroes of the COVID-19 response
The past year was exceptionally demanding on health workers, and existing workforce shortages were exacerbated by the need to respond to COVID-19, along with limited supplies of personal protective equipment, and health care worker infections.
To support the alignment of health workforce investments with current and future needs, health labour market analyses were conducted in seven countries22. In Namibia for example, the results were used to increase the health sector budget allocation to recruit unemployed doctors and nurses.

Ten-year health workforce strategic plans were launched by the Southern African Development Community (SADC) and by South Africa and Namibia. SADC Member States used the strategy to commit to investing in skills and job creation for health by increasing the fiscal space dedicated to health by 40% compared to the current baseline. Ghana revised its human resources for health strategy and developed a scheme of service for the Ghana Health Service, explaining the roles, expectations and career pathways of health workers.
To improve the availability of health workforce data, 11 countries23 implemented national health workforce accounts (NHWA). In Chad a multisectoral committee was established to analyse the relevant data, and models of care were developed to improve access to quality services at all levels of the health system.
Eritrea developed guidelines and implemented a mechanism for regulating health professions to improve the standard and quality of practice. Rural pipeline programmes are underway in Guinea and Niger, for training health workers locally and creating job opportunities towards improving retention in rural and underserved areas.
Psychosocial support to health workers responding to COVID-19
The psychosocial impact of the pandemic on health workers who have worked under extreme stress, lost colleagues and loved ones, and suffered stigma in communities is a foreboding challenge across the Region.
With support from WHO, several countries have promoted mental well-being and stress management among health workers responding to COVID-19. For instance, the Gambia provided training on WHO psychological first aid to about 900 health and extension workers, including from civil society and community-based organizations. Benin, Ethiopia and Zimbabwe trained and supported health workers and psychologists on the use of guidelines to promote self-care and provide care for patients with mental health issues. Sierra Leone created a psychosocial support pillar as part of its COVID-19 response operations to raise awareness among health workers and the population.
Mental health issues faced by health workers and the psychosocial support they receive remains an evolving area. We urge Member States to work closely with WHO and other partners, to monitor and provide the needed support to all health workers as part of the response and recovery post-COVID-19.
Building sustainable financing systems and ensuring financial risk protection
As a priority during the pandemic, countries were supported to make the case for reallocating available funding to response activities. This included evidence generation on funding modalities and public financial management challenges.
In collaboration with the West African Economic and Monetary Union, a pool of 28 experts and civil society organizations were trained on the use of the OneHealth Tool for costing implementation of strategic plans. They then supported costing of sector strategies in Côte d'Ivoire, Equatorial Guinea and Mozambique.
Eleven countries24 produced national health accounts and in Côte d'Ivoire the results have led to the introduction of a 2.5% tax on revenue from tobacco marketing, which is earmarked for the fight against AIDS.
An assessment of the efficiency of health systems in the Region was undertaken to generate evidence on ways to create fiscal space for health. Recommendations include strengthening governance, aligning incentives to outputs, improving the functionality of existing infrastructure and addressing physical and financial barriers to service utilization.
A health financing tracker for African countries was also developed. This will facilitate annual reporting against indicators, for presentation to African Union Ministers of Finance and Heads of State.
- Democratic Republic of the Congo, Equatorial Guinea, Ethiopia, Mali, Mauritius, Senegal and Zimbabwe.
- Chad, Côte d’Ivoire, Mauritania, South Africa and United Republic of Tanzania
- Botswana, Burundi, Cameroon, Gabon, Eritrea, Mozambique, Rwanda and Togo
- Côte d’Ivoire, Eswatini, Ghana, Lesotho, Mozambique, Sierra Leone, Sudan, Tanzania and Zimbabwe
- WHO recommendations on antenatal care, Antenatal care recommendations adaptation toolkit, Health worker roles in providing safe abortion care and post-abortion contraception, WHO consolidated guideline on self-care interventions for health: sexual and reproductive health and rights
- Ghana, Cote d’Ivoire, Ethiopia and Malawi.
- Ethiopia, Ghana, Malawi, Nigeria and Sierra Leone.
- Cote d’Ivoire, Ethiopia, Ghana, Kenya, Malawi, Nigeria and Sierra Leone.
- Cote d’Ivoire, Ghana, Malawi, Nigeria, Sierra Leone and Uganda.
- Cabo Verde, Comoros, Guinea-Bissau, Madagascar, Mauritius, Sao Tome and Principe, and Seychelles
- Mauritania, Niger, and Sierra Leone.
- Burkina Faso, Democratic Republic of the Congo, Guinea, United Republic of Tanzania and Togo.
- Loua A, Kasilo OMJ, Nikiema JB, et al. Impact of the COVID-19 pandemic on blood supply and demand in the WHO African Region. Vox Sanguinis. 2021 Feb. DOI: 10.1111/vox.13071 - Available at (https://onlinelibrary.wiley.com/doi/full/10.1111/vox.13071)
- Benin, Burkina Faso, Cameroon, Côte d'Ivoire, Eswatini, Gabon, Kenya, Lesotho, Madagascar, Malawi, Mauritius, Mozambique, Namibia, Rwanda, South Africa and Uganda.
- Benin, Burkina Faso, Burundi, Cameroon, Congo, Chad, Côte d'lvoire, Democratic Republic of the Congo, Ghana, Guinea, Kenya, Mali, Niger, Nigeria, Rwanda, Senegal, United Republic of Tanzania, Togo, Zambia and Zimbabwe.
- Benin, Burkina Faso, Côte d'lvoire, Guinea-Bissau, Mali, Niger, Senegal and Togo.
- Burundi, Central African Republic and Niger.
- Angola, Burundi, Cabo Verde, Cameroon, Central African Republic, Chad, Congo, Democratic Republic of the Congo, Equatorial Guinea, Gabon, Guinea-Bissau, Mozambique and Sao Tome and Principe.
- Benin, Ghana, Nigeria, Sierra Leone, Togo and Uganda.
- Cameroon, Nigeria, Senegal, United Republic of Tanzania, Uganda.
- Phase II trials in Burkina Faso, Democratic Republic of the Congo, Guinea, Madagascar, Nigeria and Togo Phase I trials in Benin, Cameroon, Ethiopia, Madagascar, Mali, Nigeria, South Africa and Uganda.
- Ethiopia, Lesotho, Mauritania, Namibia, Rwanda, Seychelles and South Africa.
- Eswatini, Ethiopia, Kenya, Malawi, Mozambique, Namibia, Rwanda, Seychelles, Uganda, Zambia and Zimbabwe.
- Burkina Faso, Côte d'Ivoire, the Gambia, Guinea, Liberia, Mali, Mauritania, Niger, Nigeria, Sierra Leone and Uganda.


