Report of the Regional Director - Executive Summary
Report of the Regional Director - 2021 - Executive Summary

Executive summary
This report of WHO’s work in the African Region between 1 July 2020 and 30 June 2021, comes at a time when health and health emergencies are in the global spotlight. The need for a strong, effective, results-driven and accountable WHO has never been greater.
Creating the WHO that we all want
Sustaining and capitalizing
on gains against polio
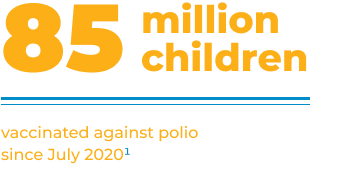
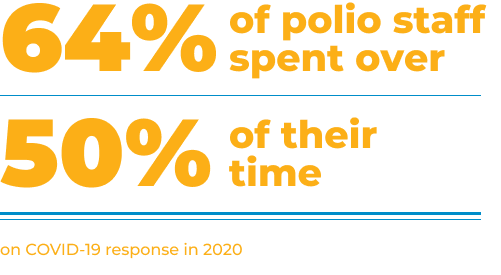
Wild poliovirus has now been kicked out of Africa after a 25-year struggle. Investments are needed to finish polio once and for all, by ending outbreaks of circulating vaccine-derived poliovirus type 2 and maintaining post-certification surveillance. More than 85 million children have been vaccinated against polio since July 2020. Hundreds of polio staff are playing key roles in the COVID-19 response, including the vaccine roll-out, as well as supporting the delivery of other high-impact health interventions.
Fighting COVID-19 and other crises
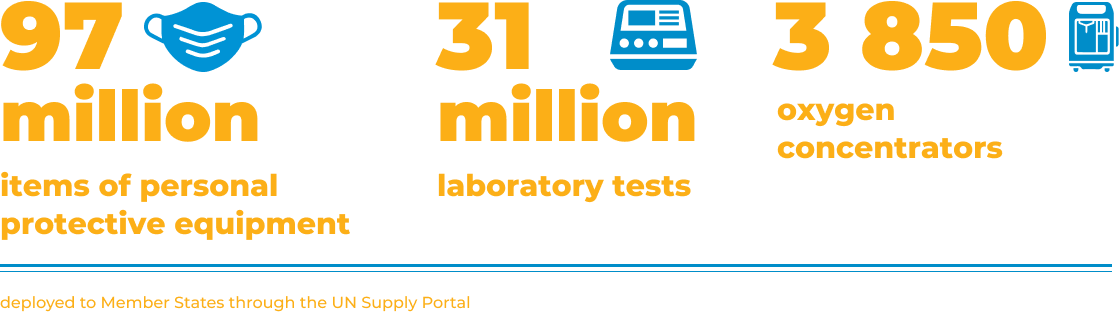
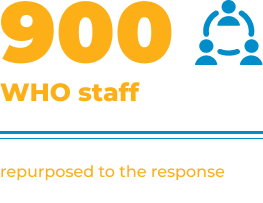
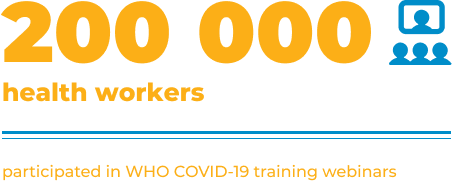
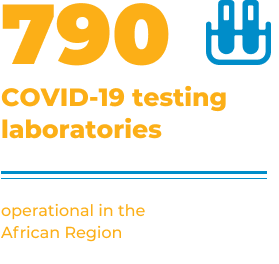
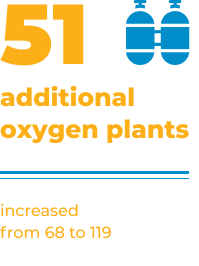
To support national authorities in leading the charge against COVID-19, WHO has been in a constant response mode. Amid global supply chain disruptions, huge quantities of essential commodities have been procured for African countries, using the UN Supply Portal, coordinated by WHO. Diagnostic and clinical care capacities have been dramatically scaled up and hundreds of thousands of health workers have been trained in key response areas.
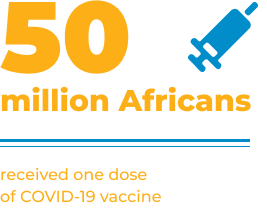
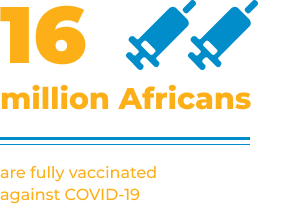
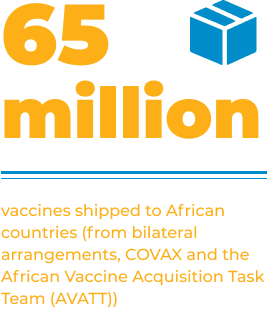
While there were delays in rolling out COVID-19 vaccines due to global inequities, this time was used to plan and prepare thoroughly, enabling several countries to race ahead quickly in using the vaccine doses when they arrived. So far, more than 65 million vaccine doses have been shipped to the African continent, including 25 million through the COVAX Facility. More than 50 million doses have been administered in African countries.

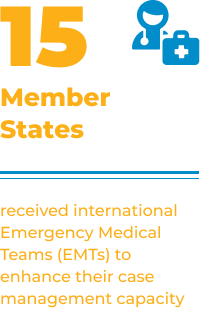
COVID-19 was one of 50 public health emergencies in response to which WHO supported countries, deploying more than 2000 experts. These include the swift control of outbreaks in Guinea and the Democratic Republic of the Congo, where experience from past epidemics was mobilized and vaccination was quickly rolled out to save countless lives. Support was also provided to vulnerable communities in humanitarian crises in northern Ethiopia and Mozambique. We have also invested continuously in readiness capacities to comply with the International Health Regulations, including strengthening Integrated Disease Surveillance and Response (IDSR). Massive demands for information to detect acute health events and inform response operations have been managed using agile approaches, new tools and by leveraging partnerships with academic institutions.
Key achievements in the COVID-19 response in the African Region

Reaffirming the need for
resilient health systems
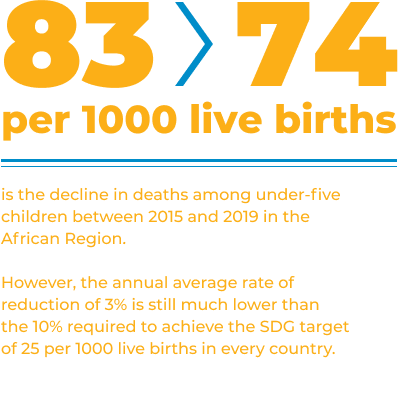
Disruptions to essential services and barriers to accessing quality care are threatening progress in priority areas. WHO has assisted countries to monitor service access and utilization and supported the implementation of a range of approaches to overcome bottlenecks. More broadly, we have guided countries on implementing integrated approaches to improve the efficiency and quality of services needed by communities throughout the life course.
The Regional Reproductive, Maternal, Newborn, Child and Adolescent Health Technical Advisory Group was launched in November 2020 to guide accelerated action to prevent deaths among mothers and children. The evaluation of a six-year effort to boost sexuality education in East and Southern Africa showed increased political will, youth mobilization, and a decrease in new HIV infections among young people in recent years.

Countries have invested in improving access to quality-assured medical products,including through the pooled procurement initiative for Small Island Developing States. Momentum towards local production has rapidly increased. Understanding of the prevalence of substandard and falsified medicines has improved, and clinical research on traditional medicines has been scaled up.
To compensate for the immense demands on front-line health workers during the pandemic, some countries have offered incentives such as insurance and transport allowances. Health labour market analyses and health workforce accounts are among the strategies being used to make the case for sustainably addressing workforce shortages. In Namibia and other countries, this has translated into additional allocations in health sector budgets for recruitment.
WHO has also supported countries through evidence generation and use of costing tools to reallocate funds to COVID-19 response operations and to expand the fiscal space for health.
Preventing and controlling diseases
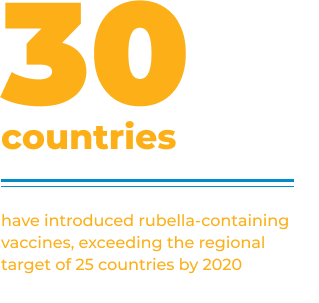
Vaccines are among the most cost-effective tools for protecting public health and through the African Vaccine Regulatory Forum (AVAREF), timelines have been expedited for these life-saving products to reach those in need. However, routine immunization coverage remains a challenge in the Region, stagnating in the past 10 years at between 70% and 75%. Strong progress in introducing rubella vaccines – exceeding the regional target for 2020 – and impressive efforts by countries to scale up supplementary immunization campaigns after disruptions due to COVID-19, indicate that with more investment, routine immunization coverage can improve. This should be a priority, to protect every child from vaccine-preventable diseases.
Eighty per cent of people living with HIV in the African Region now know their status and 70% are receiving life-saving antiretroviral therapy. TB incidence declined by 16% between 2015 and 2019, but more needs to be done to scale up access to screening for this disease. Rwanda and Uganda have established free testing and treatment programmes for hepatitis, and other countries are starting pilot projects in this direction.

The Region continues to account for 94% of the global malaria burden and overall was off track for the 2020 milestones towards elimination. Investment and innovation are urgently needed to prevent the hundreds of thousands of malaria deaths that occur every year in African countries.
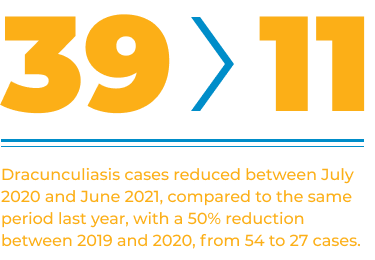
Through the Expanded Special Project for Elimination of Neglected Tropical Diseases (ESPEN) more than 221 million donated medicine tablets reached communities affected by these debilitating diseases. Countries are making progress in eliminating NTDs such as human African trypanosomiasis and trachoma.
Advancing equity and improving well-being
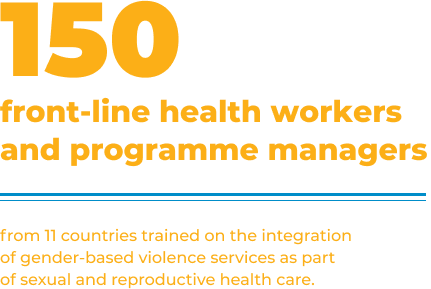
Vulnerable groups such as low-income households, women, young people, older people, ethnic minorities and people with disabilities, bear the brunt of the social and economic impacts of health crises. Health inequity analyses in 20 countries have helped to build capacities to monitor and address these disparities. For example, in response to increases in gender-based violence during the pandemic, WHO has provided policy guidance to countries and training to front-line workers.
COVID-19 has reaffirmed the need for action across sectors and for engaging all stakeholders to advance health. Collaboration with the University of Pretoria has led to the development of health-in-all-policies modules, which are being adapted and rolled out in four African universities, so that future public health experts can appreciate the value of all-of-society approaches. To improve adherence to COVID-19 preventive measures a range of tools have been developed, and community feedback is regularly collected to adjust and refine health messaging.
Vulnerable groups such as low-income households, women, young people, older people, ethnic minorities and people with disabilities, bear the brunt of the social and economic impacts of health crises.

Climate change and health projects are underway in countries to improve early warning and surveillance of climate-sensitive diseases and develop climate-resilient water safety plans. Timely support was provided to Mauritius to assess the environmental risks of an oil spill in July 2020, and in Ghana assessments of air pollution led to a report on the health and economic impacts of transport interventions in the capital city, Accra.
The International Code of Marketing Breastmilk Substitutes has now been in effect for 40 years, but only 13 countries in the African Region have enshrined the Code’s full provisions into national law. In the past year WHO has supported Kenya, Nigeria and Burkina Faso in this difficult process, which is fraught with industry interference. Overall, in the East and Southern Africa subregion, a 5% increase in the number of under-five children screened for wasting was achieved in 2020 compared to 2019, in part, thanks to advocacy and support from partners for implementing technical guidance to maintain services during the pandemic.
Support has also been stepped up to address risk factors for noncommunicable diseases. Chad, the Gambia and Mauritania have adopted regulations to introduce pictorial health warnings on cigarette packages, and Burkina Faso issued a decree to ban the sale of alcohol and tobacco within a 400-metre radius of schools during school hours. Several Member States have updated national guidelines on physical activity to integrate recent evidence, and Kenya is researching priority actions to prevent nutrition-related noncommunicable disease. To improve road safety, particularly for vulnerable groups like pedestrians, WHO is partnering with Bloomberg to support five countries to strengthen their legislation.
Integrated action and innovations for health
In cross-cutting areas such as innovation, digital health, research, laboratories, health information, primary health care and antimicrobial resistance, WHO has a dedicated team providing integrated support across technical programme areas.
A database of more than 1000 technological innovations for COVID-19 was created to improve access to information on new approaches and tools, so that countries can consider adapting and scaling them up. Kenya, Namibia and Rwanda have started preparations to introduce digital health platforms as part of strengthening information systems. The African Advisory Committee on Health Research and Development (AACHRD) supported young scientists from 20 countries to develop scientific papers related to universal health coverage and the Sustainable Development Goals.
A database of more than 1000 technological innovations for COVID-19 was created to improve access to information on new approaches and tools.

Capacity to diagnose COVID-19 was scaled up rapidly in 2020, from South Africa and Senegal being the only countries able to do so at the start of the pandemic, to all 47 countries with that capacity after a few months. Four countries introduced polymerase chain reaction testing for the first time ever with WHO support. With the development of reliable antigen-detecting rapid diagnostic tests, countries are now being urged to scale up access to these easy-to-use tools.
WHO and Africa CDC, working in collaboration, launched the COVID-19 network of genome sequencing laboratories, and support is being provided to rapidly expand genetic surveillance capacities across the continent.
There has been a tremendous amount of work under data and use of information. To better monitor health service disruptions and utilization by communities during the pandemic, a regional dashboard was created, and is being used by 27 countries, reflecting data from almost 7000 health facilities. Gaps in mortality surveillance and civil registration and vital statistics, which have been highlighted over the past year, are being addressed through the development of road maps, training and integrating the use of electronic medical certificates for cause of death.
Primary health care is central to attaining universal health coverage, and countries such as South Africa, Eswatini and Botswana have intensified action at the district level to improve the quality of care provided in communities.
Analyses of national COVID-19 clinical management protocols in African countries revealed that the majority of them recommended using antibiotics. In response, WHO has increased advocacy efforts to highlight the dangers of antimicrobial resistance and key ways of preventing it, such as evidence-based prescribing.
Communicating, coordinating
and delivering better
Partnerships with the African Union, Africa CDC, regional economic communities, the African Development Bank and other UN agencies have been strengthened through joint approaches. New private sector partners have also played important roles in supporting the response to COVID-19.
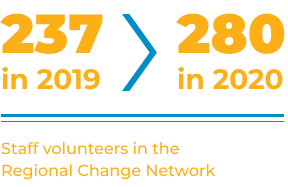
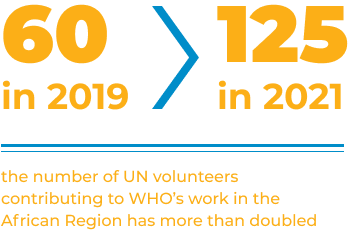
Efforts to ensure that WHO’s country offices are well-resourced have continued with the support of a dedicated group of partners. This has led to the recruitment of 22 programme management officers, 22 external relations and partnerships officers and 31 health policy, planning and coordination staff at the country level. To bridge the current funding gap for staffing, multicountry assignment teams (MCATs) are being deployed as a transitional measure to ensure Member States can readily access WHO’s technical support. We have strengthened country-level leadership by empowering WHO representatives to set priorities, coordinate, and broker for health, including engaging in UN reform and policy dialogue.

Effective resource management
The approved WHO Programme budget 2020–2021 for the African Region is US$ 992.3 million. As of 30 June 2021, the Region has used 67% of the total base funds available. To assess performance in a transparent and standardized way, the “output scorecard” approach has been introduced.
Gender parity has been reached in the WHO Executive Management Team in the Region for the first time in 2021, and through the Africa Young Women Health Champion’s Initiative, 40 young women have been recruited towards building the next generation of health leaders.
To better manage risks associated with the use of cash payments in the field, the roll-out of mobile money has been stepped up to pay over 100 000 polio campaign workers in West African countries. In the Democratic Republic of the Congo, 80 000 workers have been enrolled in a national database to facilitate future digital payments.
With the shift to teleworking during the pandemic, cloud-based services and the use of other internet applications have increased. More than 400 webinars have been convened with interpretation services. These virtual approaches have contributed to cost containment and enabled WHO to reach and engage much wider and more diverse audiences.
Challenges
Distribution of resources across WHO’s three levels also needs to be done in ways that will maximize the Organization’s impact. At the regional level, we are pursuing approaches to strengthen multicountry support, until sufficient funding is made available to allocate dedicated expertise to countries with complex settings and a disproportionate share of global health issues.
With many competing demands, prioritization is also a huge challenge, and governments and communities need to be firmly in the driver’s seat to push for changes that are evidence-based, relevant and respond to the greatest needs.
More investment is also imperative to ensure data and evidence informs policies and decisions in countries and that delivery of interventions is guided by expertise, with monitoring for quality assurance.
Looking ahead
In the year ahead, our determined effort to fight COVID-19 will continue to be a top priority, both in rolling out the vaccines and sustaining other preventive and public health measures to avoid a further resurgence of cases. At the same time, action should be prioritized to catch up on other programmes that have suffered setbacks due to disruptions induced by the pandemic, and areas where accelerated progress is needed to realize our collective goals. The principles of equity, international solidarity, and multisectoral collaboration will be key to mobilizing the needed resources and networks to improve health outcomes.
Learning from this crisis, preparedness needs to be taken up as a core element of national development and security agendas. Building on the collaboration around COVID-19, enabling environments for innovation and partnerships should also be created to facilitate all-of-society approaches towards realizing better health. The WHO Secretariat stands fy to support Member States in these areas, to make health a reality for all people in the African Region, and globally.